Topic index: A
B C
D E
F G
H I
J K
L M
N O
P R
S T
U V
W X
Z
Procedures Treatments
Home
V
Varicella | Varicose
eczema | Vasculitis | Vitiligo
VARICELLA
(CHICKENPOX)
Varicella or chickenpox is a
viral infection that causes fever and blisters which crust over
and heal after 2 to 3 weeks. It usually affects children but can
also occur in adults who may develop a more severe and sometimes
even fatal infection. The person becomes immune to further attacks
of varicella but may develop herpes
zoster (shingles) instead, later on in life.
Cause
- Varicella-zoster virus (VZV)
which is transmitted through airborne droplets, skin to skin
contact or contact with infected articles. The incubation period
is 1 - 3 weeks. After infection, the varicella-zoster virus travels
up a nerve and remains dormant (inactive) in the nerve ganglion
(nerve relay station). If activated (usually in late adult life),
the virus causes a more localised infection known as shingles
(see herpes zoster).
-
Symptoms
- Most commonly seen in children
under 10 years, but can affect any age
- Preceding fever, malaise (feeling
of illness), headache and myalgia (muscle ache).
- Pink to red spots which develop
a blister in the centre giving rise to the appearance of a "dewdrop
on a rose petal".
- The vesicles crust over a
8 to 12 -hour period.
- Usually affects the trunk,
scalp and face more than the limbs, although any part of the
body may be affected.
- The eruption occurs in crops
so that at any one time different evolutionary stages may be
seen.
- Crusts will loosen after another
1 - 2 weeks.
- Rash is itchy.
- In total, lesions take 2 -
3 weeks to clear.
 |
Varicella (chickenpox)
Click on
image for larger view |
Complications
- Scarring which increases in
the presence of secondary bacterial infection. These are often
depressed (anetoderma) but may be thickened (hypertrophic scars).
- Secondary bacterial infection
causing cellulitis, erypelas, funruncles and rarely, septicaemia
(blood poisoning)
- Pneumonia (lung inflammation).
- Encephalitis (brain inflammation),
Reye syndrome, Guillain-Barré syndrome and encephalitis.
- Disseminated infection can
occur in immunocompromised individuals and can be fatal
- Death.
- Chickenpox in pregnant women
carries additional risks for both mother and child.
- Severe chickenpox in pregnant
mothers with increased risks of varicella pneumonia and other
complications.
- Congenital varicella syndrome
may develop if infection occurs in the first 3 months of pregnancy,
resulting in an underweight baby with eye and brain abnormalities,
shortened limbs, skin scarring, cataracts and growth retardation..
Infection with varicella in the later stages of pregnancy can
cause premature delivery or neonatal chickenpox infection. This
is particularly serious if the mother becomes infected 7 days
before birth
'
- What you can do
- You should consult a doctor.
- Take antihistamines
to relieve itching.
- Avoid scratching as it encourages
secondary infection and scarring.
- Apply cool compresses.
- Apply calamine lotion to reduce
itching.
- Stay in isolation. Varicella
is infectious 5 days before the onset of the rash until all the
eruptions have crusted.
- Take paracetemol for fever
relief. Do not take aspirin as this has been associated with
the development of Reye syndrome, a life-threatening condition
causing brain and liver inflammation.
What the doctor may do
- Diagnosis of chickenpox is
usually made on the presence of its characteristic rash and the
presence of different stages of lesions simultaneously. A clue
to the diagnosis is in knowing that the patient has been exposed
to an infected contact within the 10–21 day incubation period.
Patients may also have prodromal signs and symptoms.
- Laboratory tests are often
undertaken to confirm the diagnosis.
- PCR detects varicella virus
in skin lesions and is the most accurate method for diagnosis.
Culture of blister fluid is time consuming and is less frequently
performed.
Serology (IgM and IgG) is most useful in pregnant women, or prior
to prescribing immune suppression medication to determine need
for pre-treatment immunisation.
For most healthy patients with chickenpox symptomatic therapy
is usually all that is required.
- Prescribe oral acyclovir or
valcyclovir which helps to reduce the severity of symptoms and
hasten healing
- Prescribe topical or oral
antibiotics for secondary bacterial infection.
- Give post-exposure prophylaxis
in immunocompromised persns, pregnant women <20 weeks and
newborns using Varicella zoster immune globulin (VZIG)
- After 20 weeks of pregnancy
woman can be offered oral antiviral treatment.
Prevention
- A vaccine is now available
to prevent varicella.
TOP
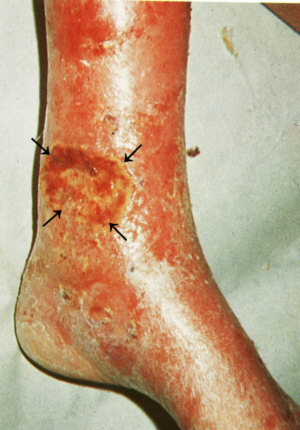
VARICOSE
ECZEMA
Varicose eczema or stasis dermatitis
is a form of eczema that occurs on the legs of patients with chronic
venous insufficiency. Women are more likely to be affected because
they have a higher risk of developing varicose veins. It may be
a precursor to more problematic conditions, such as venous leg
ulceration and lipodermatosclerosis
Cause
- Poor return of blood from
the leg veins to the heart due to faulty valves in the veins
due to past deep venous thrombosis or DVT or unknown causes,
results in blood pooling in the veins and back pressure, causing
fluid to collect in the tissues. An inflammatory reaction occurs.
Symptoms
- Redness, dryness and scaling,
occasionally with weeping and crusting on the lower portion of
the legs, especially on the inside of the ankles.
- Orange-brown pigmentation
of the skin results from haemosiderin deposition.
- Itching is common.
- Atrophie blanche (white irregular
scars surrounded by red spots)
Fibrosis or stiffening of the skin leading to lipodermatosclerosis
and a reversed “Champagne bottle” deformity of lower
leg (narrowing at the ankles)
- Varicose veins are usually
(but not always) present.
Differential diagnosis
Gravitational eczema is often misdiagnosed as cellulitis. Cellulitis
is nearly always unilateral, tender and has a well demarcated
edge
-
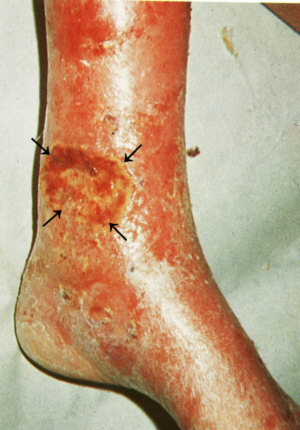 |
Varicose (stasis) ulcer.
Click on
image for larger view |
Complications
- Ulceration.
- Secondary bacterial infection.
- Allergies often develop to
topical medications used on the area.
What you can do
- You should consult a doctor.
- Avoid scratching as this may
cause ulceration and secondary bacterial infection.
- Apply saline compress
if the area is weepy.
- Take antihistamines
to reduce itch.
- Moisturise regularly
- Lose weight if obese.
- Avoid constipation by taking
high fibre diet.
- Don't stand for long periods.
- Take regular walks.
- Put up the feet as often as
possible. Raise the foot of the bed by about 10 inches to help
return blood.
- Avoid constricting garments.
- Exercise or stretch the legs
regularly.
- Wear compression bandages
or supportive stockings.
What the doctor may do
- Prescribe topical steroids.
- Prescribe antibiotics for
secondary bacterial infection.
- Conduct patch
tests to determine the cause of allergy, if necessary.
- Sclerotherapy (injections
to force closure of the varicose veins) or surgery and endovascular
laser to remove the varicose veins.
- Pinch grafts to help ulcers
heal.
-
TOP
VASCULITIS
Vasculitis refers to an inflammation
of the blood vessel walls due to an immunological reaction. It
may be localised and confined to the skin (cutaneous vasculitis)
or systemic, affecting most of the body's vasculature (systemic
vasculitis). Inflammation leads to narrowing of the lumen (channels)
of blood vessels leading to narrowing, thrombosis (clotting) or
haemorrhage, leading to ischaemia (lack of blood supply) to downstream
organs, including heart, kidneys, intestines, muscles and nervous
system. Because of their inflammatory nature, many vasculitis
syndromes are accompanied by constitutional symptoms.
The focus of this discussion
is on cutaneous vasculitis which can be classified, according
to size of the blood vessels involved into:
Small vessel vasculitis
- Cutaneous small vessel vasculitis
or CSSV (syn. leucocytoclastic vasculitis)
- Henoch-Schönlein purpura
(HSP) - (fever, arthralgias, abdominal pain, hematura)
- Exercise-induced vasculitis
- Septic vasculitis
- Small vessel vasculitis associated
with connective tissue disorders
- Urticarial
vasculitis
- Waldenstrom’s hypergammaglobulinaemic
purpura
- Mixed cryoglobulinaemia
Larger vessel vasculitis
- Polyarteritis nodosa (PAN),
which is subdivided into:
- Microscopic polyarteritis
- Cutaneous PAN
- Systemic PAN
- Granulomatous vasculitis
- Wegener’s granulomatosis
(syn. granulomatosis with polyangiitis)
- Churg-Strauss syndrome (syn.
allergic granulomatous angiitis)
- Giant cell arteritis eg Takayasu’s
arteritis (temporal arteritis is rarely associated with cutaneous
signs)
- Large vessel vasculitis associated
with connective tissue disorders
- Nodular vasculitis (syn. erythema
induratum of Bazin and of Whitfield)
Others skin conditions classified as vasculitis
- Rheumatoid nodules
- Behçet’s syndrome
- Erythema elevatum diutinum
- Granuloma faciale
- Lymphomatoid granulomatosis
- Inflammatory bowel disease
- Sarcoid
- Haematological malignancies.
- Fibrin thrombi:
present in segmented, hyalinizing vasculitis
Causes
There are many causes
of vasculitis including:
- Idiopathic, eg no cause is
identified in up to 50% of cases of cutaneous small vessel vasculitis
- Infection
- Viral - many different viruses
have been implicated including hepatitis B and C
- Bacterial - several bacterial
infections can be associated with vasculitis including streptococcal
infections (Henoch Schonlein purpura), other causes of subacute
bacterial endocarditis, meningococcal infection, and tuberculosis
(associated with some cases of nodular vasculitis)
- Medications and other drugs
- Are more likely to be associated
with small vessel vasculitis, but are occasionally associated
with systemic vasculitis
- Blood eosinophilia is noted
in up to 80% of cases with systemic involvement
- The most common drugs implicated
are penicillins, minocycline, quinolones, 'sulfa' drugs, NSAID
and other analgesics, thiazides and other diuretics, anticonvulsants,
allopurinol, vaccines, thiouracil, anticoagulants such as warfarin
and coumarin, cocaine and other illicit drugs
- Connective tissue disorders
such as lupus erythematosus
and rheumatoid arthritis.
- Abnormal proteins, either
in type or quantity eg cyroglobulins, hypergammaglobulinaemia,
hypocomplementaemia
- Inflammatory bowel disease
- Haematological, lymphoma (cancer
of the lymph glands) and other malignancies
- Physical factors eg exercise-induced
vasculitis
The mechanism of vasculitis is uncertain but is thought to occur
through the following:
- Immune complex deposition
In many vasculitis syndromes a pathogenic role for vascular deposition
of immune complexes is suspected. Consequently, many vasculitis
syndromes may be related to the prototypical immune complex disease,
Serum Sickness, and thus a form of Type III Hypersensitivity.
In some cases the complexed antigen is thought to be of exogenous
or microbial origin whereas in others it is suspected to be derived
from endogenous antigens.
- Anti-Neutrophil Cytoplasmic
Antibodies (ANCAs)
ANCAs are auto-antibodies which react with antigens in the cytoplasmic
region of neutrophils. Their presence is associated with several
vasculitis syndromes although their precise role in pathogenesis
is poorly understood. Furthermore, titers of ANCAs tend to rise
and fall with disease activity and so are useful as diagnostic
tools for management of these conditions. ANCAs are classified
according to their differential specificity to neutrophilic antigens:
- c-ANCAs stain neutrophils
in a cytoplasmic pattern and are observed in Wegener Granulomatosis
- p-ANCAs stain neutrophils
in a perinuclear pattern and are observed in Microscopic Polyangiitis
and Churg-Strauss Syndrome
Symptoms
- Purpura (haemorrhagic spots
or patches) which is slightly raised. Purpura does not disappear
when pessed.
- Blisters, painful nodules
(swellings) and ulcers may occur in more severe cases.
- Urticarial
vasculitis which
is different from ordinary urticaria
in that it lasts more than 24 hours and heals with a dark stain.
- Livedo reticularis which is a mottled or net-like bluish
or purplish discolouration of the skin. It may be a sign of polyarteritis
nodosa which may affect the skin alone (cutaneous polyarteritis
nodosa) or the skin and internal organs (systemic polyarteritis
nodosa).
- Henoch-Schonlein purpura
(HSP) is a type of
vasculitis caused by the deposition of IgA in the small blood
vessels. It characteristically presents with a triad of vasculitic
rash, joint and abdominal pains (sometimes accompanied by constipation
or diarrhoea). In some cases it may affect the kidneys, causing
haematuria (blood in the urine) and potentially, kidney damage.
The symptoms are often preceded by fever. HSP is more common
in children but adults may also be affected. It may represent
a hypersensitivity reaction caused by streptococcal throat infections.
HSP is also known as leucocytoclastic or anaphylactoid purpura.
Who gets HSP?
 |
Vasculitis.
Click on
image for larger view |
- Complications
Complications are usually caused by vasculitis affecting internal
organs, for example,
- Systemic polyarteritis nodosa
may cause fever, joint and muscle pains, nausea, vomiting, abdominal
pain, heart failure, high blood pressure, kidney problems, strokes
and nerve damage.
- Wegener's granulomatosis may
also affect the larger blood vessels, mouth, ear nose and throat
(ulcers and destruction of the nasal cartilage leading to a saddle
nose deformity), lungs (coughing of blood and breathlessness),
eye, kidney and nerve inflammation.
-
Diagnosis
- Skin
biopsy - Histology showing inflammatory infiltrate in wall
of dermal or subcutaneous vessels; may be neutrophilic, lymphocytic
or granulomatous, often red blood cell extravasation, variable
fibrinoid necrosis of vessel walls; DIF showing Immunoglobulins,
complement or fibrin in the vessel wall.
- Conduct blood, urine and other
tests to exclude involvement of internal organs.
Treatment
- Treat with systemic steroids,
dapsone, colchicine and immunosuppressive
drugs.
- Prescribe non-steroidal anti-inflammatory
drugs (NSAIDs) for pain relief.
- Treat the underlying cause,
if any.
TOP
VITILIGO
Vitiligo or leucoderma occurs
when the skin pigment, melanin is not produced. It affects about
1% of the population and is a serious cosmetic problem in dark-skinned
individuals. A familial tendency has been observed.
Cause
- Autoimmune disease (self-allergy)
in which the body's defence system mistakenly attacks the melanocytes
(melanin-producing cells) as though they were foreign.
Symptoms
- Well-defined milky white patches.
- Occurs most commonly on the
face, neck, hands, elbows, knees, the body folds such as the
armpits and groin, nipples, genital areas, around orifices (mouth,
eyes, anus, umbilicus) and on areas of trauma (eg., along scratch
lines).
- May have evidence or a history
of other autoimmune diseases such as premature greying of the
hair (see canities), alopecia
areata, diabetes, pernicious anaemia, Addison's disease and
thyroid disease.
 |
Vitiligo.
Click on
image for larger view |
- Complications
- Very occasionally, vitiligo
may spread to involve very extensive areas of skin.
What you can do
- You should consult a doctor.
- Use cosmetic camouflage.
What the doctor may do
- Exclude other autoimmune diseases
or check for antibodies to thyroglobulin and parietal cells (which
are increased in autoimmune disorders).
- Prescribe topical steroids.
- Treat with topical or oral
PUVA - natural or artificial
sunlight in association with psoralens (a photosensitising medicine
that may be applied to the skin or taken by mouth).
- Minigrafting which involves
removing circular areas of depigmented skin with a biopsy punch
and replacing them with grafts taken with the same instrument
from other sites such as the buttocks.
- Bleach the remaining skin
to a uniform white colour if vitiligo is very extensive.
- Keypoints
- The treatment of vitiligo
is not very satisfactory.
- Repigmentation is slow and
may not be complete, especially over the fingers and bony prominences.
- Repigmentation is unlikely
if the area involved has no hair follicles or the hairs there
are white.
TOP